Under the three central pillars of care, research and training, the Uganda Cancer Institute is dedicated to advancing cancer treatment. Executive Director, Dr Jackson Orem, discusses serving the nation’s oncological needs.
INTRODUCTION
Cancer is an epidemic that affects the lives of millions worldwide on a yearly basis. Across sub-Saharan Africa, the region has witnessed a 45 percent increase in the number of cancer-related deaths from 2000 to 2020, with cervical cancer representing one of the major contributors to mortality rates.
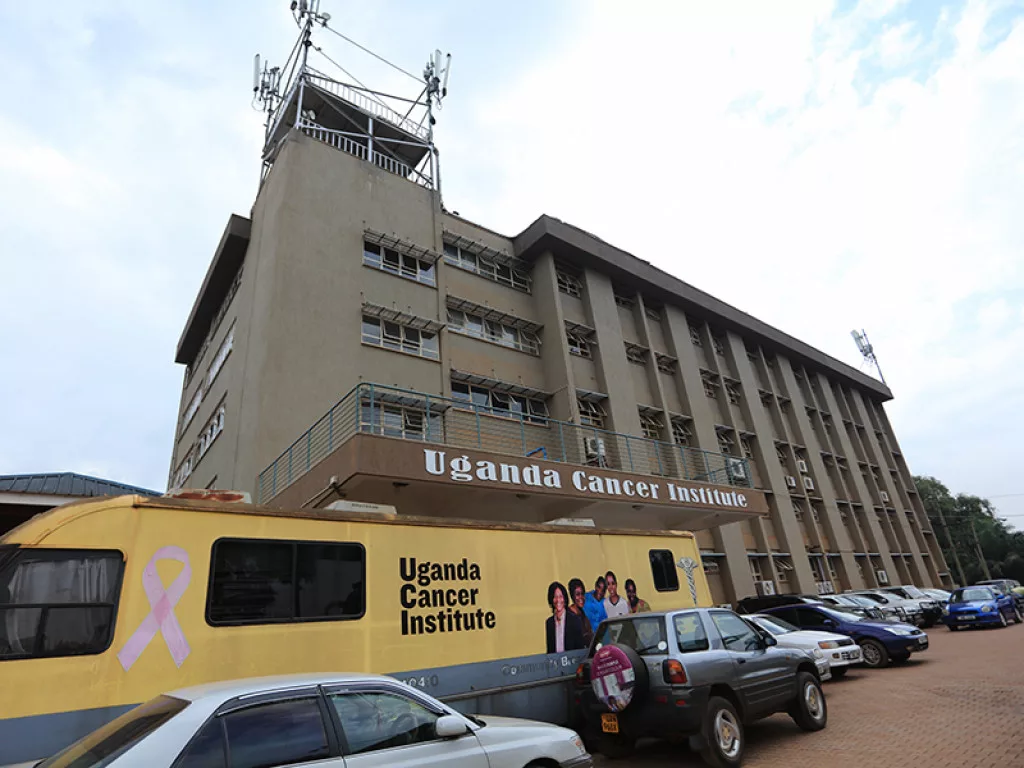
In the face of the widespread threat of this deadly disease, for over half a century the Uganda Cancer Institute (UCI) has operated as a government agency tasked with cancer care, research, and training.
Centred in Kampala, the Institute was conceived in 1967 with the development of the Lymphoma Treatment Centre (LTC) – a collaborative venture with the Makerere University medical school, the Ministry of Health (MOH) and the National Cancer Institute (NCI) in the USA.
The Institute was born from the discovery of Burkitts lymphoma, a childhood tumour initially encountered in Uganda in 1958. The discovery led to seminal research works, resulting in the Institute becoming the first dedicated cancer research centre in Africa.
Crucially, it contributed to the initial identification of a cancer-causing virus – the Epstein-Barr virus (EBV) – and shortly after, the development of experimental treatment using chemotherapy.
Under the UCI Act 2016, UCI is mandated to undertake and coordinate the management of cancer and cancer-related diseases in Uganda.
“I consider cancer in Africa as one of the underserved and neglected areas of the continent’s health sector, hence the reason for my choice of career in oncology,” opens Executive Director at UCI, Dr Jackson Orem.
“It was the passion to serve the underserved that inspired me to originally join medical school,” he continues. It is a passion that has continued to develop ever since Orem joined UCI in 1999 as an oncology registrar, and subsequently grew through the ranks.
Indeed, since its roots over half a century ago, UCI continues to further its mission by embracing new technologies and developing research centres across the country to widen the Institute’s reach and awareness. Currently, UCI is in the process of implementing four new treatment centres throughout Uganda that effectively service the entire population. As the designated East Africa Centre of Excellence in Oncology (EACEO), the construction of a new state of the art facility is also underway, due for completion later this year.
“To increase access to cancer care, the government of Uganda through UCI is decentralising cancer care services by establishing Regional Cancer Centres (RCCs) in western, north-western (West Nile), the northern, and the eastern regions,” Orem outlines.
UCI’s remit extends to oncology services within medical oncology, gynaecological oncology, surgical oncology, paediatric oncology, radiation oncology, cancer therapeutics, palliative care, diagnostics (laboratory and radiology), research and training, with palliative care services integrated throughout these main disciplines.
Advocating a comprehensive approach, the overall goal of UCI is to reduce the burden of cancer in Uganda and within the East African Community (EAC). This spans the entire continuum of cancer control, primary prevention, early detection, diagnosis and treatment, palliative care, survivorship, and surveillance.

“The vision of UCI is to become a top internationally recognised centre of excellence in cancer services”
Dr Jackson Orem, Executive Director, UCI


ADVANCING CANCER AWARENESS
The invaluable resource of research lies at the heart of UCI, as the foundation for the care solutions it develops and offers.
As evidenced by the Institute’s foundational ties with the Makerere University, educational initiatives and training programmes form a key segment of UCI’s work in Uganda. Through these schemes, UCI seeks to secure the field’s sustainability by sourcing new talent and educating future healthcare workers in the face of a significant national shortage of trained medical professionals and oncology specialists.
“Cancer care is multidisciplinary, requiring many specialists working together. Currently UCI has 254 full-time employees, of which 177 are the multi-disciplinary clinical team, including nurses.
“Although there is a steady improvement in the staffing, there is still a dire shortage of cancer specialists to adequately run the facilities.”
As Orem suggests, the limited talent pool in Uganda poses a threat to the sector’s development. To address the need for human resources, since 2017 UCI has implemented oncological fellowship training programmes to develop much-needed medical professionals in the field. These include initiatives in gynaecological, paediatric, haematological, and adult oncology.
“We host three oncology fellowship programmes in collaboration with several partners to build the national and the EAC member states’ human resources capacity for cancer control.
“Our ongoing plan is to expand these training programmes to include other specialty areas such as radiation oncology, and oncology-nursing,” he comments.
Launched in collaboration between UCI, the Makerere College of Health Sciences, Mulago National Referral Hospital (MNRH), and the Fred Hutchinson Cancer Research Centre (FHCRC) to name just a few key partners, these programmes have strategically positioned UCI as the East African Centre of Excellence and an esteemed training hub for cancer specialists across the field.
“In December 2021, UCI won the best health sector e-health service of the year, awarded by the national information technology authority (NITA) Uganda and its partners”
Dr Jackson Orem, Executive Director, UCI

EMBRACING DISRUPTIVE TECHNOLOGY
Since its beginnings, UCI’s innovative incorporation of technology has been recognised as industry leading. Most recently, the Institute was awarded the title of best health sector e-health service of the year by the National Information Technology Authority (NITA) Uganda and its partners: Ernst & Young Global Limited, Huawei Technologies Uganda, and the World Bank Uganda.
As the first stage of cancer control, early detection and information sharing are a vital part of the work that UCI do. Within this, UCI has devised a Comprehensive Community Cancer Programme (CCCP) to operate outreach services, delivering key information and detection screenings across the country’s communities.
By deploying a van equipped with a mammography unit for breast cancer screening and a separate space to screen for signs of cervical cancer, UCI extends critical services to wide-reaching and remote rural areas.
The Institute acquired its first ‘mobile mammo-unit’ in 2009, under the auspices of Yale University School of Medicine’s “Health Overseas Partnerships in Health and Education” (HOPE) programme, in partnership with Johnson & Johnson. In 2018, UCI received a second mammography-van donated by the Honorary Consul of Uganda in Mumbai, India, Madhusudan Agrawal, from the Samta Foundation and Tata Group.
“Additionally, UCI is piloting the feasibility of implementing an Interactive Voice Response (IVR) system for dissemination of cancer information via telephone calls for the purpose of cancer awareness in Uganda,” Orem tells us.
“This IVR is supported by the key cancer specialists as part of the call centre to provide tele-services.”
Through IVR, phone calls are automatically answered by a computer system that plays back audio messages and predetermined navigation instructions through voice commands or dual-tone multi-frequency signalling (DTMF).
In the realm of cancer diagnostics, UCI has invested in diagnostic devices for complete blood count, blood chemistries, tumour markers, immunohistochemistry, pathology, and conventional imaging with a computerised tomography (CT) scan. These imaging services will be further upscaled with the installation of modern Magnetic Resonance Imaging (MRI) equipment, and the establishment of a nuclear medicine centre equipped with a Single Photon-Emission Computed Tomography (SPECT) and Positron Emission Tomography (PET)/CT scanners.
“Finally in radiotherapy, in addition to the cobalt-60 teletherapy machine and cesium 137 brachytherapy unit, UCI has expanded to acquire an additional cobalt-60 teletherapy unit and a CT-simulator which was commissioned in June 2016.”
In the same year, UCI commissioned an upgrade to a high-dose rate brachytherapy unit, alongside the later replacement of Co-60 source. In 2021, UCI’s commissioning of a Truebeam Linear Accelerator (LINAC) launched the gradual transition from 2D to 3D conformal radiotherapy.
“We are adopting e-health in a phased manner where functionally, resource wise, and ethically appropriate,” Orem surmises.

AN UNRELENTING MISSION
Operating within a realm of healthcare that Orem himself describes as “complex, multi-sectorial and expensive”, the work that UCI does is rife with challenges. Alongside rising numbers of cancer cases, the Institute must weather insufficient funding compared with national need, the prohibitive cost of training abroad for specialists facing few opportunities in-country, and the aforementioned lack of cancer care specialists.
Nevertheless, Orem identifies an advantageous shift in the health care sector that will only bring further development.
“This is an area that has a lot of potential for improvement, given the growing burden. Policies in developing countries are now changing, since for a long time the emphasis has been on communicable diseases, not cancer.”
With this optimism at the fore, UCI remains laser-focussed on its strategic priorities for the year ahead.
“This includes fast-tracking the operationalisation of the four regional cancer centres, and the finalisation and approval of the national cancer control plan.
“We will also be strengthening UCI’s existing local training programmes and expanding to include other specialty areas, whilst developing local and international partnerships for domestic manufacturing of the key high-volume cancer care supplies, including anti-cancer medicines,” he continues.
UCI will continue to navigate these challenges and lead the way in fulfilling its mandate on behalf of the wellbeing of all Ugandans.
























